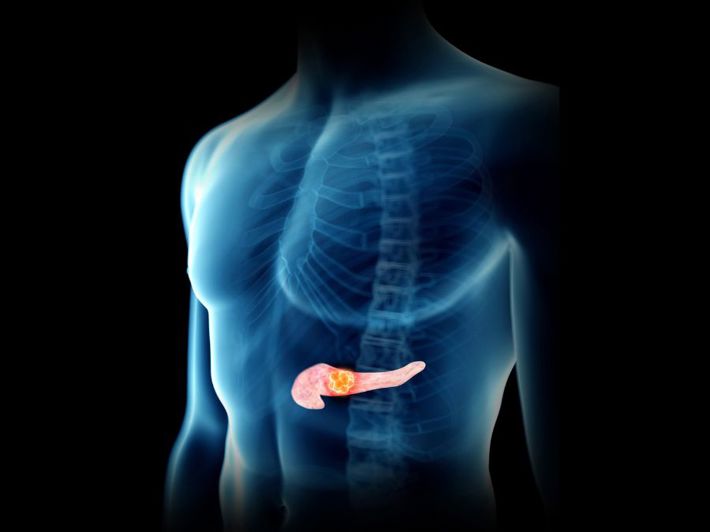
Pancreatitis usually occurs due to gallstones. There are two main types of pancreatitis: acute and chronic. Both types are serious and can lead to complications.
Acute pancreatitis usually resolves within a few days with proper treatment, while chronic pancreatitis lasts longer and worsens over time if untreated, causing permanent damage to the body. [1]
What are the symptoms of pancreatitis?
Both acute and chronic pancreatitis share pain in the upper abdomen, which may radiate to the back, accompanied by nausea or vomiting. However, the nature of the pancreatic pain may differ between the two types. [2]
Symptoms of Acute Pancreatitis
- Sudden and severe pain in the upper middle abdomen.
- Pain may radiate to the back.
- Usually begins 12–24 hours after a fatty meal.
- Pain intensity ranges from mild to very severe.
- Lasts for several days.
- May be accompanied by other symptoms, such as fever, nausea and vomiting, rapid heartbeat, malaise, and extreme fatigue.
Symptoms of Chronic Pancreatitis
- Pain in the upper abdomen, which worsens especially after meals.
- Pain may radiate to the back.
- Pain can be intermittent or continuous.
- Pain may disappear for a while as inflammation progresses over time.
- Some patients may not feel any pain or symptoms until complications develop later.
- May be accompanied by other symptoms, such as diarrhea, foul-smelling oily stools, nausea and vomiting, weight loss due to malabsorption, and high blood sugar.
When should you see a doctor?
Go to the emergency room immediately if you have severe, unbearable abdominal pain that prevents you from sitting or finding a comfortable position.
See a doctor as soon as possible if you experience sudden abdominal pain that does not improve over time or is accompanied by the symptoms above. Leaving pancreatitis or similar conditions untreated can lead to serious health risks and complications. [3]
The Digestive Diseases Department at Al Ahli Hospital has an experienced and highly skilled medical team capable of accurately diagnosing and treating various gastrointestinal conditions, including pancreatitis and similar disorders. Contact us for more information.
How is pancreatitis treated?
Most cases of acute pancreatitis improve with hospital treatment and rest. Patients may need to stay in the hospital for a few days under supervision to receive intravenous fluids, antibiotics, and pain relievers as needed. In more severe cases, treatment may involve addressing the underlying cause of inflammation, which can include gallbladder removal, abscess drainage, removal of damaged pancreatic tissue, or repair of any bile duct problems. [4]
For chronic pancreatitis, treatment aims to relieve the patient’s pain, restore pancreatic function, and prevent serious complications.
Depending on the case, this may include: [4]
- Pain relievers.
- Following a low-fat diet.
- Enzymes to aid digestion.
- Nutritional supplements to compensate for vitamin deficiencies caused by malabsorption.
- Insulin injections to reduce high blood sugar.
- Surgery in some cases.
Chronic pancreatitis is a persistent disease; pain may worsen or temporarily disappear then return, which can cause frustration and depression. Therefore, it is important to consult a doctor for advice on managing these challenges, which may include: [4]
- Following the doctor’s instructions carefully.
- Planning a healthy low-fat diet in consultation with a certified nutritionist.
- Drinking plenty of water, as pancreatitis can cause dehydration.
- Quitting smoking, alcohol, and other harmful habits.
- Attending psychological counseling if feeling depressed to cope and adapt better.
Exercising, improving sleep quality, and practicing relaxation techniques to reduce stress and anxiety caused by the condition.